INTRODUCTION
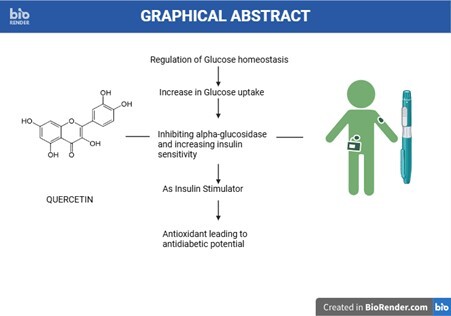
The most popular dietary flavonoid is quercetin, a polyphenol with a pentahydroxy flavone chemical structure. With five hydroxyl groups located at positions 3, 3,', 4,', 5, and 7 (Michala & Pritsa, 2022), the C ring (Figure 1 ) is a heterocyclic pyrene to which two benzene rings, A and B, are linked. The presence of the hydroxyl group facilitates easier interaction with metal ions and results in antioxidant properties (Nagori, Nakhate, Yadav, Ajazuddin, & Pradhan, 2023), which is the structural trait that sets this flavonoid apart from others. According to metabolic research, all four of the hydroxyl groups—aside from the one at position five—participate in the glucuronidation process, which is catalyzed by the enzyme UDP-glucuronosyltransferase (Manman et al., 2019) and proceeds through a Phase II metabolic pathway (Boersma et al., 2002) with the assistance of isoforms. They include UGT1A1, UGT1A8, and UGT1A9 exhibiting both competitive and non-competitive inhibition, resulting in the production of quercetin conjugates like glucuronides, which are vital in influencing the bioavailability of the compound (Zhang et al., 2021). The percentage of quercetin that is available in the bloodstream is contingent upon the consumption of fruits, vegetables, and fruit juices, such as grape juice, onions, and apples, respectively (Kaşıkcı & Bağdatlıoğlu, 2016). With ingesting grape juice, the bioavailability varied by 1.4%, whereas with apples and onions (Dávalos, Castilla, Gómez-Cordovés, & Bartolomé, 2006), it was closer to 30%. Plasma vitamin C, the sugar moiety in quercetin glycoside, solubility, and interindividual variables like sex differences (Hai et al., 2020) are additional factors that increase the bioavailability. After consuming foods high in quercetin, the amount present in the plasma varies between 28 to 142µM (Dabeek & Marra, 2019). These secondary metabolites have pharmacological uses in treating diabetes, arthritis, bladder infections, cancer, and inflammation, but there is still a lack of conclusive scientific data (Batiha et al., 2020; Maalik et al., 2014). The antioxidant qualities of quercetin in human plasma are dependent on its concentration. Lower concentrations lead to antioxidant qualities that are affected by proton and electron transfer (Qi, Qi, Xiong, & Long, 2019), pH, catechol groups, and the signal transduction pathway as well as enzyme-related activities. Similarly, a meta-analysis (Bule, Abdurahman, Nikfar, Abdollahi, & Amini, 2019) study found that quercetin lowered serum glucose levels at dosages of 10, 25, and 50 mg/kg. It has been discovered to enhance insulin sensitivity and decrease blood glucose levels in glycaemic management (Haddad & Eid, 2017). Quercetin was found to act in a fashion similar to that of the first-choice antidiabetic drug metformin by controlling diabetes mellitus through the AMP-activated protein kinase signalling pathway (Dhanya, Arya, Nisha, & Jayamurthy, 2017), which enhances glucose uptake and metabolism. It is also a key regulator of cellular energy homeostasis (Chellian, Mak, Chellappan, Krishnappa, & Pichika, 2022). They play a crucial role in enhancing glucose uptake, inhibiting gluconeogenesis, and regulating metabolic pathways involved in glucose metabolism (Shen et al., 2022) ).Other ways that quercetin works include controlling blood sugar levels, promoting the uptake of glucose in skeletal muscles when insulin is not present, blocking the enzyme glycogen phosphorylase, which increases the synthesis of glycogen and controls glucose homeostasis and boosting insulin secretion from pancreatic β-cells. A study on isolated aortas of streptozotocin-nicotinamide diabetic-induced rats demonstrated that quercetin's synergistic effects on the administration of anti-diabetic medications, including metformin, reversed endothelial damage. Aiming to lower the risk factors of diabetes such as atherosclerosis, myocardial infarction, and coronary diseases (Petrie, Guzik, & Touyz, 2018), combined quercetin and metformin therapy was found to improve the lipid profile, decrease triglycerides and total cholesterol, and reduce serum levels of low-density lipoprotein and high-density lipoprotein. Previous studies have investigated the combination of quercetin and resveratrol in reversing hyperglycemia (Yang & Kang, 2018). In a similar vein, quercetin and liraglutide have demonstrated a possible synergistic effect (Eraky, Ramadan, El-Magd, & F, 2021), while quercetin and gliclazide have demonstrated promising clinical outcomes in the treatment of diabetes (Abdelkader et al., 2020).
This review aims to understand the mechanistic pathways by which quercetin holds the potential to maintain serum glucose levels with an emphasis on its antioxidant properties. In addition, the clinical studies enhancing antidiabetic potential in combination with marketed diabetic drugs highlight the need for natural therapies as an adjuvant treatment.
QUERCETIN AS ANTI-DIABETIC AGENT
REGULATION OF GLUCOSE HOMEOSTASIS
Skeletal muscle and liver play a crucial role in maintaining peripheral glucose homeostasis through the use of Insulin and glucagon, two peptide hormones that regulate glucose levels in the human body. The skeletal muscles account for 80% of postprandial glucose uptake, while the liver is responsible for 80% of its release. Quercetin interacts with various molecular targets in the pancreas, liver, skeletal muscles, adipose tissue, and small intestine to maintain cellular homeostasis. It does this through multiple pleiotropic mechanisms, including reducing glucose absorption, increasing insulin secretion, and promoting glucose utilization in peripheral tissues (Ansari et al., 2022).
INCREASE IN THE UPTAKE OF GLUCOSE BY QUERCETIN
The use of Quercetin has been found to result in a 1.5-fold increase in glucose uptake, which is comparable to the effect of insulin, according to a study conducted by (Haddad & Eid, 2017). This study demonstrated that flavonoids activate GLUT-4, the insulin-responsive glucose transporter that is present in intracellular vesicles in the basal stage and is translocated to the plasma membrane in the fed state, thereby increasing glucose uptake. This translocation process is mediated by the Phosphoinositide 3-kinases (PI3K) pathway and the 5’-AMP protein kinase (AMPK) regulatory enzyme, which is also known to stimulate GLUT4 translocation. Quercetin has been shown to increase the cell surface content of GLUT4 receptors, increase the content of GLUT4 protein in L6 myotubes, and increase AMPK and glucose transport (Haddad, Eid, Nachar, Thong, & Sweeney, 2015). Additionally, the antidiabetic potential of Quercetin lies in its ability to regulate glucose homeostasis in the liver, which maintains equilibrium between the processes of gluconeogenesis, glycogenesis, and glycogenolysis. Activation of AMP reduces the activity of the enzyme G6Pase involved in hepatic glucose production processes, and it has been found that Quercetin can reduce hepatic glucose.
INHIBITING ALPHA-GLUCOSIDASE AND INCREASING INSULIN SENSITIVITY
Alpha-glucosidase is a membrane-bound enzyme located in the small intestine playing a crucial role in the breakdown of disaccharides into oligosaccharides and glucose absorbed into the bloodstream (Zhao et al., 2022). Inhibitors of the enzyme delay the absorption process reducing postprandial glucose levels and marketed drugs acarbose, voglibose, and miglitol are reported with gastrointestinal side effects like abdominal cramps, flatulence, and liver disease that hinder its use. As an alternative, quercetin is identified to be a natural alternative with lower side effects (Kato-Schwartz et al., 2020). In a recent study conducted by (Shen et al., 2022) estimating the inhibitory kinetics and isolation of active components from the green walnut husk, quercetin showed an inhibitory potential of IC50 values of 92.87µg/ml. It is found to follow a non-competitive inhibitory mechanism in the reduction of glucose. (Proença et al., 2017) discuss on the structural relationship of quercetin responsible for causing glucosidase inhibition. The presence of hydroxyl group at the 5,7 or 8th position (A ring), 3’ and 4’ hydroxylation’s (B ring), 3rd position (C ring), and the double bond between C2 to C3 is critical to enumerate the glucosidase inhibitory activity that is reported by an in-vitro study conducted alpha-glucosidase inhibition by the flavonoids. (Xing, Chun, Qiang, Xiong, & Rui-Hai, 2021) had elucidated the mechanism of the metabolite quercetin-3-O-glucronide and its inhibitory potential by exhibiting reversible and mixed mode of inhibition through the formation of complexes between quercetin and alpha-glucosidase catalyzed by hydrogen bonding and van der Waals forces that Favors enzyme microenvironment. This study suggests that quercetin has the potential to interact with alpha-glucosidase and necessitate inhibitory processes.
QUERCETIN AS INSULIN STIMULATOR
It activates L-type Calcium channels Cav1.3 present in the β-cells of islets of Langerhans stimulating insulin release. The influx of Ca2+ ions triggers exocytosis in insulin-containing vesicles and opens dihydropyridine-type sensitive L-type Ca2+ channels allowing for the secretion of insulin (Tuluc, Theiner, Jacobo-Piqueras, & Geisler, 2021). Quercetin mediates the voltage sensitivity of the channels and enhances the intrinsic efficacy of glucose. BayK8644 is a calcium channel agonist and a chemical compound targeting voltage-gated calcium channels and quercetin acts at a site different from Bayk8644 in acting as an insulin secretagogue (Bardy et al., 2013). Further, it was found to inhibit ATP-sensitive potassium channels in a study conducted on rat insulinoma INS-1 cells through the acute application of quercetin (Kittl et al., 2016).
ANTIOXIDANT EFFECT LEADING TO ANTIDIABETIC POTENTIAL
Quercetin acts as a strong antioxidant by scavenging free radicals and binds transition metal ions that protect the body against oxidative damage. It increases the intracellular levels of glutathione (GSH) activating the MAPkinase signaling pathway. The production of free radicals during metabolic processes in the body is linked to the development of associated diseases such as heart, liver, and diabetes (Asmat, Abad, & Ismail, 2016). Destruction of pancreatic beta cells that produce insulin is linked to the production of reactive oxygen species and other processes by which free radicals lead to diabetes include oxidation of glucose, protein glycation and degradation of glycated proteins (Yorek, 2003). The imbalance caused by high levels of free radicals and declined antioxidant enzyme levels leads to cell damage, inactivation of enzymes, and lipid peroxidation (Bajaj & Khan, 2012) . The power to combat oxidative damage by quenching free radicals involves signalling pathways like MAPK, NFκB, and AMPK and regulation of antioxidants such as catalase, and glutathionase. It acts as a strong antioxidant by scavenging free radicals and binds transition metal ions. Figure 2 reveals the mechanistic pathway of quercetin's role in acting as an antidiabetic.
MOLECULAR TARGETS OF QUERCETIN INTERACTION
The superior efficacy of the flavonoid quercetin in reducing diabetes involves targeting pathways that either increase the uptake of glucose in skeletal muscle, utilize glucose, enhance the transport of glucose and insulin signalling, inhibit α-glucosidase and α-amylase, suppress inflammatory cytokines, etc.
AMP-ACTIVATED PROTEIN KINASE PATHWAY
AMPK regulates the metabolism of glucose and lipids with a reference to changes in energy status. It is a crucial regulator of energy homeostasis and acts as a sensor detecting the ratio of AMP/ATP monitoring the cellular energy (Świderska et al., 2021). In a low energy level, AMPK is activated and triggered executing a range of downstream effects promoting the uptake of glucose from muscle and adipose tissue, enhancing glucose metabolism in the liver, decreasing glucose production, accelerating metabolism of lipids, and increasing storage of glucose. This process reduces sensitivity towards insulin and reduces resistance to insulin. By regulating the glucose levels, it reduces the oxidative stress and inflammation. It has control over the hormone regulation of insulin, glucagon, and leptin (Kakoti, Alom, Deka, & Halder, 2024).
Quercetin binds to the AMPK α subunit in the activation of the enzyme AMPK. The catechol moiety 3,4-dihydroxy phenyl located in the B ring is crucial for binding towards the enzyme. The presence of five hydroxy groups is essential for binding and the ring system A and B with a heterocyclic C ring provides a scaffold for binding. The affinity of quercetin towards AMPK is increased by the planar structure enabling a pi-pi stacking interaction with the aromatic residues. The specific binding site is located in the allosteric drug and metabolic site (ADaM), which is a hydrophobic pocket in which reversible and competitive binding such as AMP occurs (Dhanya et al., 2017). Upon binding it increases the AMP/ATP ratio increasing the glucose uptake in the skeletal muscles. It activates calcium-calmodulin mediated protein kinase beta (CaMKKβ), liver kinase B1 (LKB1), and upstream kinases (transforming growth factor-β-activated kinase 1 (TAK1)), that phosphorylates and activate AMPK. It has the potential to inhibit AMPK inhibitors such as protein phosphatase 2A (PP2A) and maintain the energy status. It acts similarly to metformin in bypassing insulin-regulated systems for GLUT4 translocation.
PI3K/AKT Pathway
Phosphotidylionistiol 3-kinase belongs to a family of enzymes present in the plasma membrane and plays a crucial role in cell signaling processes such as glucose uptake in metabolically active tissues like adipose tissues, skeletal muscles, and liver. They are GLUT4 translocators and PI3K generates phosphatidylinositol 3,4,5-triphosphate (PIP3) that recruits AKT and activates AKT phosphorylates leading to GLUT4 translocation (Świderska et al., 2021). The transfer from intracellular storage sites to plasma membrane enhances glucose uptake. Quercetin regulates glucose levels by inhibiting PI3K/AKT phosphorylation and downstream the insulin signaling processes reducing glucose uptake and metabolism. It also involves pro-inflammatory signaling pathways.
DPP-IV inhibitor
Quercetin has been identified to show potential in the inhibition of the Dipeptidyl peptidase-IV enzyme, which breaks down incretin hormones such as Glucagon-like peptide-1 and is involved in glucose metabolism and insulin secretion. By acting as an inhibitor, it maintains GLP-1 levels enhancing insulin secretion and maintaining glucose tolerance. They improve pancreatic β-cell function and prevent the degradation of glucose-dependent insulinotropic peptide (GIP) increasing the secretion of insulin. Though it is claimed with supreme efficacy in acting as a DPP-IV inhibitor, further human studies are essential to explore its therapeutic potential (Ansari et al., 2022).
ROLE OF INHIBITION IN ADVANCED GLYCATION END (AGE PRODUCTS)
In hyperglycaemic conditions, the reducing sugars interact with amino acids undergoing the Maillard reaction resulting in the formation of AGEs. It can also be formed through non-enzymatic processes and a polyol pathway that turns glucose into fructose. The generation of AGEs leads to associated symptoms that damage the kidney (diabetic nephropathy), retinal vasculature (diabetic retinopathy), the nerves (diabetic neuropathy), the skin, and underlying tissues (diabetic foot ulcers). The potency of quercetin in inhibiting protein glycation surpasses the synthetic drug aminoguanidine. The antioxidant, anti-inflammatory, and antihyperglycemic properties inhibit the formation of AGE-products, methylglyoxal, and glyoxal improving diabetic complications (Alam, Ahmad, & Naseem, 2015).
GPX4 (glutathione peroxidase 4) and Quercetin
GPX4 is highly expressed in tubular epithelial cells and its level is a predictor for renal outcomes, ferroptosis (antioxidant role in lipid peroxidation), and patients with diabetic kidney disease (DKD) are associated with (Wang, Chang, Zhao, & Chen, 2022) where increased urinary protein, serum creatinine, estimated glomerular filtration rate, and the percentage of sclerosed glomeruli in renal specimens. It further induces oxidative stress by increasing generating ROS production. An increased expression of GPX4 is seen with quercetin which can activate GPX4 enzyme activity enhancing its antioxidant properties. It has been found to protect against oxidative stress, inhibit ferroptosis, offer renal protection, show synergistic action, regulate cell signaling, and improve insulin sensitivity to maintain glucose levels.
STIMULATING INSULIN THROUGH m TOR PATHWAY
The mechanistic target of Rapamycin is another target of quercetin and modulates the activity of mTORC1 signaling cascading the downstream pathways. The free radicals scavenging capacity of quercetin increases the AMP/ATP ratio activating the mTOR signaling pathway and triggering for secretion of insulin in a dose-dependent manner (Dhanya & Kartha, 2021). The treatment with quercetin induces mitochondrial biogenesis, leading to the synthesis and secretion of insulin from pancreatic β-cells which are released by hypertrophy due to change transient change in ATP/AMP and mitochondrial potential enhancing insulin secretion. Figure 2 illustrates the pictorial representation of the targets unveiling quercetin’s interaction leading to a reduction in glucose levels.
Bioavailability of Quercetin
The absorption site for QE is in the small intestine, where a major portion gets absorbed and a minor proportion in the stomach. The QE in the lumen of the intestine passes through the epithelial cells to reach the systemic circulation. The health benefits of quercetin depend on its absorption in the digestive system and its bioavailability in the human body (Kaşıkcı & Bağdatlıoğlu, 2016). In most quercetin-rich foods, the sugar molecule is attached to quercetin and the conjugate is a glycoside. Based on the food material, the glycosidic attachment differs and affects its bioavailability. To cross the gut component, quercetin depends on the size and polarity of the glycoside and the previous studies support that onion-derived glycoside quercetin is highly bioavailable and causes greater absorption (Kato-Schwartz et al., 2020) . QC has a very low oral bioavailability due to its water-insoluble property that limits its clinical application as a therapeutic agent. The hydrophobic nature allows it to permeate through the phospholipid layer whereas, the mucus layer is surrounded by water content of up to 90% that prevents its passage via the mucus to reach the intestinal cells and absorbed (Kittl et al., 2016). Quercetin enters into enterocytes and blood is rapidly metabolized. Improving the hydrophilicity of quercetin through alteration of structural parameters and nano-formulations helps to increase the bioavailability.
COMBINATION THERAPIES OF QUERCETIN WITH ANTIDIABETIC DRUGS
CLINICAL STUDIES OF QUERCETIN WITH GLICLAZIDE
(Abdelkader et al., 2020) studied the in-vivo effect of combining gliclazide, a second-generation sulfonylurea-based anti-diabetic drug with the natural agent quercetin possessing anti-oxidant and anti-diabetic effect. Gliclazide acts by binding to the sulfonylurea receptors (SUR) situated on the β cells of the pancreas and acts by closing the ATP-dependent potassium channels that lead to an influx of calcium ions and releasing insulin by process of exocytosis. Though gliclazide acts as an insulin secretagogue, repeated exposure to sulfonylurea therapy leads to a decrease in the insulin reserve, thereby leading to a decline in efficacy. Combination therapies prove to be a good choice and quercetin, a dietary flavonoid has been explored for antidiabetic potential in preclinical studies. The study conducted by the research team on a streptozotocin-induced experimental model of diabetes on 60 adult male albino Wistar rats and administration of gliclazide (10mg/kg,p.o) and quercetin (50mg/kg.p.o). The findings of the study suggested that coadministration of gliclazide along with quercetin reduces blood glucose levels and also causes for reduction in the C-peptide levels to maintain the lipid profile. The mechanism attributed to quercetin includes hindering cholesterol synthesis leading to anti-atherogenic potential (Abdelkader et al., 2020).
QUERCETIN AND METFORMIN
In a recent study by (Chellian et al., 2022) streptozotocin-nicotinamide-induced diabetic rats were studied for the synergistic effects of quercetin and metformin. The dosage induced included quercetin of 10mg/kg and metformin of 180mg/kg in its combination. The endothelial dysfunction of the isolated aorta was examined through the conduct of ex-vivo studies, identifying the plasma glucose and lipid levels through histological studies of the liver, kidney, pancreas, aorta of the abdomen, and thorax. Although quercetin and metformin are found to possess antidiabetic activity in unison and their mechanism is found to be unclear, the combination therapy exhibits synergistic effects. This research emphasizes that the endothelium acts as a permeable barrier between two components, the blood bloodstream and vascular wall maintain the tone of the vesicles. Hyperglycaemia is associated with dyslipidemia and alterations in the cardiovascular tone, and combination therapy offers a range of pharmacological activity by lowering plasma glucose and improving liver gluconeogenesis and lipid parameters. Though the mechanism for these processes, remains unclear, it is hypothesized that restoration of genes in glucose/lipid metabolism, enzyme alterations in the liver, and rendering immunity or protecting inflammation in the cardiovascular system would be an additive contributor to this therapeutic approach. An alternative genetic association is evident with STZ-induced nicotinamide injection.
QUERCETIN AND SITAGLIPTIN
(Eitah et al., 2019) explored combination therapy of herbal remedy with gliptins in diabetic management. This study was conducted with quercetin (50mg/kg) and sitagliptin (70mg/kg) on STZ (45mg/kg i.p) induced diabetic rats (110 adult male Wistar rats). A part of the study estimated the dosage of Sitagliptin capable of reducing plasma glucose level and it was calculated to be at 70mg/kg. Similarly, in another part of the study, animals were grouped into four groups, with Group I (animals receiving tween 80), Group II (Diabetic rats without any treatment), Group III (Administration of Sitagliptin at 70mg/kg,p.o), Group IV (Combined therapy of Sitagliptin and Quercetin). The histopathological studies were conducted by sacrificing the animals and collecting the samples directly from the heart and storage at -80°C with the estimation of biochemical parameters. The previous studies report that administration of sitagliptin increases the C-peptide in serum which is essential for the synthesis of insulin, the current study shows that combination therapy has the potential to restore C-peptide. Furthermore, the reduced ROS and lipid peroxidation levels, increased serum SOD and GSH levels, and decreased cholesterol and triglycerides preserve the integrity and architecture of β-cells thereby reducing apoptosis. The herbal adjuvant quercetin exerts protection by exhibiting antioxidant, anti-apoptic, and anti-inflammatory effects.
QUERCETIN AND LIRAGLUTIDE
(Gaballah, Zakaria, Mwafy, Tahoon, & Ebeid, 2017) investigated the effectiveness of combination therapy quercetin and liraglutide in high-fat diet STZ-induced diabetic rats and estimated parameters like hyperglycemia, unfolded protein response stress markers (UPR) in the prevention of oxidative stress leading to inflammation. The study included the usage of sixty male albino rats divided into five groups, Group 1 and 2 being the normal (citrate buffer) and diabetic control respectively, Group 3 and 4 consisting of Liraglutide and Quercetin treated diabetic model, Group 5 with a combined treatment of Liraglutide and Quercetin. The period of the study included 4 weeks and quantitative measurements of blood glucose, insulin, serum inflammatory protein, XBP1 mRNA PCR analysis, Bcl-2 and Bax levels, and redox parameters such as tissue malondialdehyde (MDA), glutathione levels (GSH), advanced oxidation protein products (AOPPs) were assessed. The combined treatment was found to protect beta cells, UPR, and ER stress-induced apoptosis and inflammation. Table 1 indicates the combination of quercetin with current antidiabetic drugs acting by different mechanisms and streptazotocin-induced animal studies further show their efficacy in reducing blood glucose levels in type 2 diabetic rats/mice.
Table 1
Antidiabetic drugs in combination with the bioflavonoid quercetin in strepatazotocin induced diabetic rats/mice in reduction of blood glucose levels.
CONCLUSION
Natural therapies such as adjuvant combinations have been explored in recent days and with flavonoids consumed in our daily dietary intake, quercetin holds great potential in the treatment of diabetes mellitus. As a dietary supplement, the holistic ways by which this secondary metabolite enumerates a series of anti-diabetic, anti-oxidant, anti-apoptotic, and anti-inflammatory activities are explored in the current era to understand the predictive mechanistic pathway. In this review, we focussed on the anti-diabetic potential of quercetin and highlighted the chemical structure of this particular flavonoid with its five hydroxyl groups playing a crucial role in binding to AMPK, PI3K/AKT, DPP-IV, m TOR pathways thereby increasing the intracellular receptors causing for GLUT4 translocation, increasing the cell surface content of GLUT4 receptors that accelerates range of physiological pathways such as insulin secretion, glucose uptake and sensitization. The molecular targets by which quercetin regulates anti-diabetic activity involve inhibition of advanced glycation end products, GPX4, and stimulation of m TOR receptors in the reduction of glucose levels. Since the bioavailability of quercetin limits its uptake in the small intestine as it is hydrophobic, several formulation methods are in current research to increase its content in systemic circulation. Furthermore, in-vitro studies are being carried out in various laboratories, mostly using streptozotocin-induced diabetic rat/mouse models and four antidiabetic drugs explored include metformin (biguanides), sitagliptin (DPP-IV inhibitors), liraglutide (incretin mimetics) and gliclazide (sulfonyl urea receptors). The findings instigate quercetin to act as an adjuvant therapy in alleviating symptoms such as hyperglycaemia, and hyperlipidaemia, and decrease ROS production acting as an anti-oxidant, anti-diabetic, and anti-inflammatory. Further, human clinical trials on effects of quercetin as hypoglycaemic agent are lacking and needs to be explored for understanding its efficacy as anti-diabetic agent. This study will lay a pathway in the evaluation of quercetin's potential to combat cardiovascular diseases and to act as an anti-apoptotic agent in the treatment of cancer.