INTRODUCTION
The COVID-19 pandemic is unparalleled in human history. Accompanied with the normal viral side effects, this infection showed multiple organ damage, such as severe cardiovascular damage, shock, and syndrome of acute respiratory distress (Chen et al., 2020; Wu & Mcgoogan, 2020). The new coronavirus severe acute respiratory syndrome coronavirus 2 causes Covid-19. Perishing because of SARS CoV 2 has wreaked havoc on so many lives around the globe, making it the most notably catastrophic pandemic disaster since World War II (Li, 2016). As they can easily mutate and recombine to adapt to new situations, coronaviruses are responsible of effectively altering host’s machinery and tissue growth.Coronaviruses encompass a vast assemblage of RNA viruses characterised by their single-stranded nature, which mostly induce respiratory ailments and, to a lesser extent, gastrointestinal disorders. Respiratory manifestations induced by coronaviruses encompass a spectrum of presentations, ranging from symptoms akin to the common cold or mild influenza to more serious manifestations such as pneumonia. Observational study designs have demonstrated that death rates are elevated among the older population, whereas the prevalence of such occurrences is considerably lower among children (Lu et al., 2020).
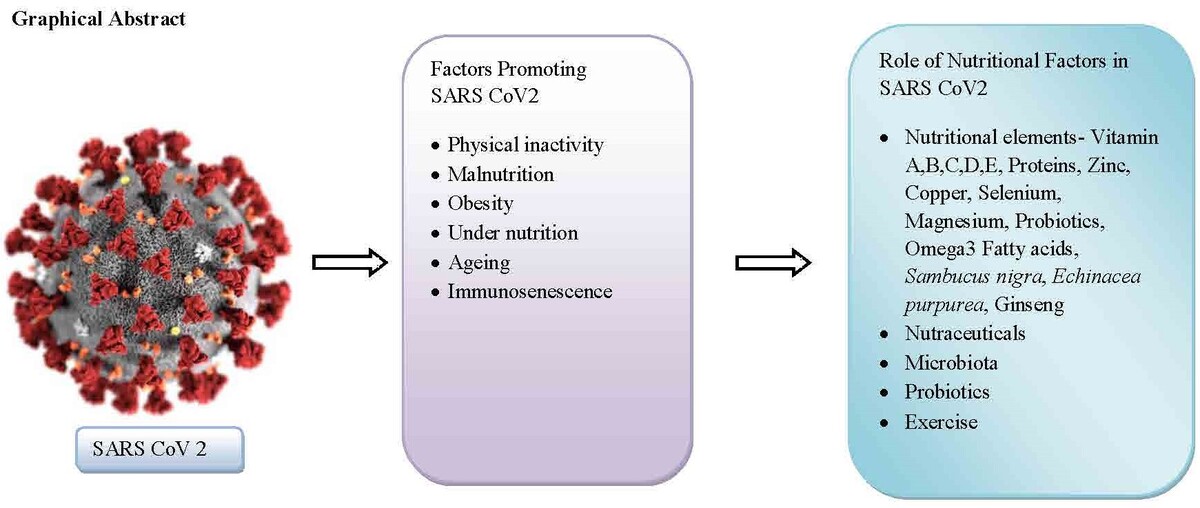
SARS-CoV-2 is a recently discovered human coronavirus, representing the seventh known member of this viral family. It is characterized by its novelty and the unfamiliarity of the immune system in humans with this disease. Thus, the lack of protection to this virus has aided its rapid spread and severe sickness. This particular illness has been designated as coronavirus disease discovered in 2019 (Covid-19). Strong immune systems are essential to preventing infectious illnesses, as demonstrated by the implications of Covid-19 and SARS-CoV-2 on health, society, and the economy. Insufficient immune responses have become an essential health hazard in areas where they were previously ignored or accepted. The immune system is directed and strengthened by vaccines to fight a specific infection. The observed efficacy of the recently produced Covid-19 vaccines serves as an indication of the underlying vulnerability of some subpopulations' immune systems. However, it is important to note that vaccinations need a strong immunological response in order to function effectively. This article examines the impact of various factors on the human immune system, including infection with SARS-CoV-2, aging, malnutrition, obesity, intestinal microbiota, complications related to nutritional deficiency, and nutritional recommendations (Calder, 2021).
METHODOLOGY
In order to carry out this research, an exhaustive search of the relevant scholarly literature was conducted across a number of different repositories, including Web of Science, Springer, Nature, Science Direct, Scopus, and PubMed. The search focused on identifying papers that documented research pertaining to both preclinical and clinical aspects throughout the timeframe spanning til the year 2023. The research utilised the phrases "SARS-Cov2”, "nutrition," “Immune system”, "nutrients," “Obesity”, "dietary need," "nutraceuticals," "Covid-19," "Coronavirus." We systematically eliminated any publications that were not directly relevant to the precise topics of interest.
PHYSICAL INACTIVITY AND COVID-19
In order to modulate immunological responses against several viral infections, it is important to maintain a balanced dietary intake (Curtis et al., 2017). Insufficient nutritional intake and an unwholesome dietary pattern have been found to considerably compromise the immune system's functionality, hence augmenting the vulnerability to infectious diseases (Childs & Calder, 2019). There is a correlation between pandemic-related isolation measures and a rise in calorie intake as well as a decline in physical activity, which is particularly concerning given that both of these factors raise the possibility that Covid-19 may have a more severe result (Gallo, Gallo, Young, Moritz, & Akison, 2020). Physical inactivity has a deleterious influence on immune system function, muscular strength, metabolic function, body weight, and haemostatic variables, especially in middle-aged and older adults. Engaging in moderate activity, as opposed to strenuous exercise, has been found to improve immunological processes, leading to a reduced occurrence of upper respiratory tract infections (Bull & Hardman, 2017). The influence of a suboptimal dietary pattern on susceptibility to corona virus infection, as well as its subsequent outcomes such as severity, recovery, and the likelihood of re-infection across various patient groups, has been found to be substantial (Jayawardena & Misra, 2020). A host's ability to defend itself against viruses is weakened by diets robust in sugar, processed carbohydrates and saturated fatty acids, but lacking in fibre and antioxidants (Milanski et al., 2009). Previous studies have observed that foods containing high levels of saturated fats can result in continuous activation of the innate immune system's defensive mechanisms, while simultaneously inhibiting adaptive immunity. Saturated fatty acid-rich meals do, in fact, have a major effect because they induce lipotoxic conditions that can activate TLR 4 on neutrophil and macrophage outer membranes, thereby continuously stimulating the innate immunological response. Consequently, this process has the potential to activate other pathways involved in inflammation and stimulate the synthesis of proinflammatory molecules (Milanski et al., 2009; Rogero & Calder, 2018). Diet affects the activity of the toll-like receptor (TLR9) which has been linked to a catastrophic Covid-19 result in individuals at risk. Obesity and a high-fat diet, or HFD, cause rats and humans to have elevated TLR9 upregulation in the visceral fat cells (Thomalla et al., 2019). By activating macrophages and increasing plasmacytoid dendritic cells (pDCs), high fat diet (HFD) causes an excess synthesis of nucleotides and associated regulatory antigens, exacerbating cellular inflammation (Revelo et al., 2016). In animal studies, high-fat-diet induces an augmentation in the infiltration of macrophages into both the lung cells and alveoli. The elevated incidence of lung epithelial cell inflammation as well as the alveoli’s injury observed in corona affected individuals who are obese and have signs of metabolic syndrome may be caused by a similar mechanism (Dias, Joyce, Postel-Vinay, & Xu, 2020). Additionally, carbohydrates, sweets, and diet rich in fats might increase oxidative stress. This, in turn, hinders the division and differentiation processes of both T and B cells, ultimately leading to death. Consequently, this collective effect suppresses the immune system's adaptive response to viral infections.
In experimental models using animals, it was observed that a diet rich in fats exacerbated pulmonary damage as well as extended the immunological adaptive response in cases of influenza infection. This study found reduced memory T cell activity, circulating antigen response, and influenza virus clearance (Green & Beck, 2017). The precise mechanisms responsible for the elevated lung damage remain uncertain, but it is plausible that programmed cell death may be implicated. Thus, aged, comorbid, and Covid-19-risk persons should avoid bad diets that may worsen the disease. Dietary nutrients, minerals and vitamins, and perhaps even rare microorganisms like probiotics are all important components of an immune-supportive, well-balanced diet. Proteins, vitamins, and minerals have long been recognised as significant contributors to overall health and immunological homeostasis, thereby crucially boosting infection resistance. A recent comprehensive systematic review regarding impact of dietary habits on the body's reaction to respiratory infections caused by viruses, mineral and vitamin intake are important for mounting an immune protection against the infection and are linked to how severe the infection develops. Adipose tissue comprises many cells that produce angiotensin-converting enzyme 2, or ACE 2, so since obese people have more adipose tissue, they may have more angiotensin-converting enzyme 2. ACE 2 represent a protein receptor towards corona virus in host cells, and the virus has been found to exhibit an increased affinity for angiotensin-converting enzyme 2 (ACE2) (Shubina et al., 2020; Wang et al., 2019; Zhang et al., 2020; Zheng & Kanneganti, 2020). Normalizing nutrition and body weight with habits, medicinal substances, and surgical strategies reduces the risk of metabolic, inflammatory diseases and pulmonary (Mey, Kirwan, & Axelrod, 2023).
OVERVIEW OF IMMUNE SYSTEM ROLE AND ORGANISATION
The primary role of the defense framework in a human being is to shield the person by eliminating dangerous microbes. In order to effectively defend against a diverse range of infectious agents, the immune system of human beings has undergone evolutionary adaptations that encompass a multitude of cellular components, several signalling molecules, and multiple functional reactions. The body's defense system has four primary functions. First and foremost, it functions as a protective barrier that prevents the infiltration of microorganisms into the human body. Additionally, the immune system functions by detecting microorganisms and determining their potential for damage. Moreover, the immune system functions by effectively eradicating microorganisms that have been recognized as detrimental, which entails the destructive activities carried out by diverse immune cells. In addition, it is worth noting that the immune response elicits immunological memory, hence leading to a heightened and expedited immune response upon subsequent exposure to the pathogenic microorganism, surpassing the magnitude and swiftness of the first reaction. The ability to perform intricate and advanced activities is possible due to the diverse array of cell types present throughout the immune system of an individual, each possessing unique functional capacities. These various cellular entities interact reciprocally as part of the response of organism achieving effective pathogen defense measures are implemented for optimum safety (Calder, 2021). The body's defenses may be categorized into several classifications, with the most prevalent being natural and acquired immunity. The role of immunity in establishing antiviral capability is presented in Figure 1.
Figure 1
Summary of immunity against viruses- CTL, cytotoxic T lymphocyte; NK, natural killer cell; MHC, major histocompatibility class; IFN, interferon; TLR, Toll-like receptor;NFκB, nuclear factor kappa-light-chain-enhancer of activated B cells; Th, helper T lymphocyte; B cell, B lymphocyte cell; Ig. Immunoglobulin; IL, interleukin; TNF, tumor necrosis factor.

IMAPCT OF AGEING ON IMMUNE SYSTEM
Immunosenescence—a reduction in immunological function—is commonly associated with aging (Agarwal & Busse, 2010; Montgomery & Shaw, 2015; Pawelec, Larbi, & Derhovanessian, 2010; Pera et al., 2015). The characteristics of immunosenescence encompass a disrupted equilibrium of immunoglobulins, reduced quantities of T cells (in blood), decrease in naïve B lymphocytes, imbalances among various phenotypes, a decrease in non-functional memory B cells, a generation of inactive memory T lymphocytes, diminished diversity of antigen receptors, weakened responsiveness, impaired growth, and reduced cytokine generation, including interferon (IFN)-γ and interleukin (IL) 2. Furthermore, dendritic cells exhibit reduced reactivity, diminished production of type 1 interferons, reduced Toll-like receptors upregulation as well as impaired phagocytic activity. Neutrophils, natural killer cells, and macrophages demonstrate impaired phagocytosis, reduced cytokine output, and altered Toll-like receptor (TLR) expression. Immunosenescence reduces bone marrow production, the body's main source of immune cells. Aging causes thymic complication, resulting in decreased naïve T cell generation and reduced immunological responsiveness to new antigens. Immunosenescence refers to the phenomenon wherein older individuals exhibit heightened vulnerability to diseases, such as respiratory illnesses including pneumonia, compared to younger people (Fulop, Pawelec, Castle, & Loeb, 2009; Goodwın, Vıboud, & Sımonsen, 2006). Additionally, older individuals tend to have diminished immune responses to immunization. The intestinal mucosa is often regarded as the body's major site of immunological tissue. Studies conducted on murine models have shown that the gastrointestinal mucosal immune response undergoes senescence, characterized by decreased immunoglobulin A secretion, gastrointestinal sensitivity to new antigens, and mucosal antigen presenting cell (dendritic cell) activity. It is believed that advanced age may serve as a possible trigger that increases the vulnerability of the elderly individuals to experiencing more severe signs of Covid-19. Ageing paradoxically increases blood levels of numerous inflammatory mediators, causing inflammageing. This state increases the risk of chronic age-related diseases such as heart diseases, diabetes, neurological diseases,non-alcoholic liver disease, and some cancers. Additionally, individuals in this state may be more prone to experiencing an exaggerated infection-induced inflammation. The immunological system's innate response requires inflammation for body defence. However, an overactive inflammatory response can negatively impact acquired immunity (Fujihashi & Kiyono, 2009; Ogra, 2010).
MALNUTRİTİON AND SARS COV2
Malnutrition is characterised by an insufficient intake of calories, micronutrients and macronutrients. Micronutrient deficiency is a shortage of essential nutrients needed for growth. Individuals may be overfed in terms of calories yet lacking in one or more micronutrients in their regular diet, despite the seeming contradiction. Inadequate consumption of essential nutrients is now widespread, resulting in decreased infection resistance and ultimately an increase in illness severity (Calder, Carr, Gombart, & Eggersdorfer, 2020). Nutrition is essential for immune system support. A healthy diet regulates immune homeostasis exceptionally effectively. According to (Calder et al., 2020) an appropriate dietary routine is essential for defending against viral dangers. Currently, it's possible that the immune system's effectiveness has been compromised by shifts in food and lifestyle patterns, mostly as a result of social isolation. Indeed, even slight deficits or deficiencies of some essential nutrients might affect immunological response (Bhaskaram, 2001; Calder et al., 2020). Vitally, this may be reversible if the patient's dietary status is enhanced. Disease prevalence and mortality have been found to be negatively correlated with dietary intakes of key micronutrients as vitamin B12, iron, vitamin D, and vitamin C, especially in community subsets predisposed to vitamin malnutrition due to genetics. However, worldwide COVID-19 results are expected to be impacted by the widespread global prevalence of starvation and deficiency in essential elements (Fedele, Francesco, Riso, & Collo, 2021).
In a study employing a cross-sectional design, (Li et al., 2020) found that 52.7% of patients were undernourished. One well-known risk factor is malnutrition that has been linked to worse health outcomes such hospitalisation duration, mortality, and readmission (Agarwal et al., 2013). According to Anker et al. (2020), COVID-19 patients have significant weight loss, perhaps to the point of developing cachexia, which is characterized by a lack of both muscle and fat. Numerous dietary and metabolic aspects contribute to Covid-19 weight loss, including higher body warmth, reduced appetite, and heart and kidney issues. A study by (Rouget et al., 2021) found that 37.5 percent of Covid-19 patients were malnourished according to the standards set by the Global Leadership Initiative on Malnutrition. Thirty-eight of fifty covid-19 people tested at a prominent centre in South Korea had insufficient levels of vitamin D, and twenty one possessed inadequate zinc levels (Im et al., 2020). Relative to control group, twenty-four percent of corona virus infected patients possessed severely deficient vitamin D levels. The study suggests that proper nutrition is crucial for maintaining respiratory health. Identifying and treating dietary deficits in respiratory patients is crucial. In addition, 78.9% of those who weren't having trouble breathing were nonetheless considered to be malnourished. The overall data indicated that vitamin D insufficiency was quite common, and that all seriously sick patients lacked more than one essential nutrient. Using serum albumin, lymphocyte count and total cholesterol as its basis, the controlling nutritional status index was recognised as a determinant of risk for mortality in Corona virus affected patients. Serum albumin levels may be a good indicator of the condition's severity. (Wu et al., 2020). Malnutrition and undernourishment are, therefore, conditions that can aggravate the severity and outcome of the illness; inspite of that on the flip side, being infected with covid-19 causes a condition that causes malnutrition and weight loss (Barazzoni et al., 2020). A single-center examination of 109 individuals (Recinella et al., 2020) found that elderly covid-19 patients with severe nutritional vulnerability died more often. According to Pironi et al., 2021, half of hospitalized covid-19 individuals reported malnourished and 70% of those patients were above the age of 65. Saturated fatty acid, sugar and refined carbohydrate-heavy diets, as well as those poor in dietary fiber, anti-oxidants, disturb the sensitive adaptive-innate immune balance, weakening the host's ability to fight off invading pathogens (Milanski et al., 2009). These diets are also related with a delayed rate of recovery from a Covid-19 infection as well as an increased frequency of severe acute respiratory syndrome caused by corona virus 2 (Butler & Barrientos, 2020). Chronic innate immune activation is triggered by saturated fatty acid-rich diets, whereas adaptive immunity is suppressed. In certainty, macrophage and neutrophil surface toll-like receptors TLR4 might be activated by a high saturated fatty acid diet, constantly stimulating the natural defense mechanism. Proinflammatory mediator synthesis and activation of additional pro-inflammatory pathways of communication may result from this (Rogero & Calder, 2018). It has been hypothesised that a poor diet could lead to the highly serious consequence of covid-19 in susceptible individuals by altering both the level of expression of TLR9 and the amount of intrinsic stimuli for TLR9 activation (Thomalla et al., 2019). TLR9 expression in mouse and human visceral adipose tissue is elevated by a high-fat diet and obesity (Bezemer & Garssen, 2021). Through macrophage activation and liver plasmacytoid dendritic cell growth, high-fat diet increases metabolic inflammation by producing excess nucleic acids and associated protein antigens (Revelo et al., 2016). The immune system relies on a nutritious diet that provides it with the micro and macro nutrients, minerals, vitamins, and maybe even probiotics, that it needs to function properly (Zabetakis, Lordan, Norton, & Tsoupras, 2020). The effects of vitamins, minerals, and proteins on immunological homeostasis have long been considered crucial to good health and immunity to infections. Vitamins and minerals may affect covid-19 severity and mortality. Trace elements, Vitamin B-complex, E, C, D helps the immune system stay stimulated (Carr & Maggini, 2017; Zuo et al., 2020). Consequently, vitamin and mineral composition deficiencies may exacerbate Sars-cov2 infections.
OBESITY AND SARS COV2
Numerous physiological processes might account for the correlations of COVID-19 infection and obesity severity and likelihood that have been found. The condition of long-term over-nutrition gives rise to obesity, a condition that is autonomously linked to compromised metabolic rate, breathing capacity, and inflammation. These characteristics are recognized as risk elements that contribute to increased disease severity (Mey et al., 2023). Patients with covıd-19 have exaggerated and life-threatening reactions of inflammation, or “cytokine storm,” because macrophages, particularly common immune cell in fat tissue, get activated. Within flu affected individuals, inflammatory mediators such tumor necrosis factor and plasma interleukins (IL-8, IL-15, IL-6) caused unfavorable outcomes and were more increased in fat patients compared to healthy patients (Hagau et al., 2010). This finding may be generalizable to the Covid-19 scenario. A past investigation found that increasing visceral adiposity and intramuscular fat deposition independently and significantly correlate with critical signs among individuals receiving treatment of covid19. Excessive intramuscular fat accumulation and visceral obesity were also identified to be predicted associated with risk for mechanical ventilation; the second factor also raises the likelihood of dying. High levels of both visceral adiposity and intramuscular factor were shown to be independent unfavourableprognostic variables for rapid covıd-19 disease development, supporting the authors' previous findings (Yang et al., 2020) similar findings were seen in a retrospective research involving covıd-19 patients in Italy. A high lung severity score indicates the patient is suffering from severe interstitial pneumonia, and other key indicators include visceral fat, C-reactive protein, age, and lactate dehydrogenase. High lung severity score and visceral adipose tissue were shown to be independently associated with the requirement for intensive care, as were rising lymphocytes, D-dimers, and abdominal fat. This confirms that visceral adipose tissue is an unfavourable prognostic factor (Watanabe et al., 2020). Obesity is thought to worsen covıd-19 disease regardless of age, gender, or conditions. In animal studies, high-fat diet enhances lung tissue and alveolar macrophage infiltration. In persons with metabolic syndrome or obesity suffering from corona virus infections, an analogous working may result in inflammation of the lung epithelial cells and damage to the alveoli (Dias et al., 2020). Furthermore, the consumption of a diet that is rich in carbohydrates and high in fat has been found to result in an increase in oxidative stress, which slows B cell and T cell proliferation and maturity while also inducing apoptosis, all of which contribute to a diminished adaptive immunological response to viral infection (Green & Beck, 2017). A high-fat diet increased damage to the lungs and delayed the adaptive immune reaction within animal studies of influenza infection. This inhibited memory T cell activity, antigen presentation, and influenza virus clearance. Programmed cell death may cause lung injury (Shubina et al., 2020; Wang et al., 2019; Zhang et al., 2020; Zheng & Kanneganti, 2020). Hence, it is advisable for those aged 65 and over, those with underlying health conditions, and individuals susceptible to covid-19 to exercise prudence, as the consumption of inadequate foods may potentially increase the probability of experiencing severe manifestations of the virus. The magnitude of the covid-19 pandemic symptoms has been linked to impaired metabolic health. Intermittent fasting has potential in terms of metabolism and obesity, rendering it a captivating nutritional strategy with hypothetical implications for COVID-19 (Mey et al., 2023). Community efforts should be directed towards reducing the incidence of obesity as well as overweight and increasing the frequency of healthy eating and frequent physical exercise.
OBESITY, MICROBIOTA AND COVID-19
Probiotics are exogenous bacteria and yeast products found in processed foods, pharmaceuticals, and nutritional supplements. Probiotics protect floral variety and gut health. Probiotics boost immunity and minimize viral illnesses, especially viruses that affect the respiratory tract (Mey et al., 2023). Previous studies have linked obesity to changes in gut bacteria. These microorganisms encompass fungal, viral, bacterial, and archaea, which are single-celled microorganisms. Collectively referred to as the gut microbiota, obese individuals have been found to exhibit reduced variety and abundance in the composition of bacteria (Chatelier et al., 2013; Graessler et al., 2013; Ley, Turnbaugh, Klein, & Gordon, 2006). As stated earlier, the presence of gut bacteria is crucial for safeguarding against pathogenic germs, regulating the immune system, and performing essential processes including digestion, metabolism, and short-chain fatty acid synthesis. Around 90% of microbes are firmicutes and bacteroidetes. Several studies have indicated a greater proportion of firmicutes as to bacteroidetes in the faecal samples of individuals with obesity. Emerging research findings indicate the existence of microorganisms, namely bacteroidetes, firmicutes, and proteobacteria, within the pulmonary system. Furthermore, a reciprocal association has been observed between the lungs and the gastrointestinal tract (Aziz, Doré, Emmanuel, Guarner, & Quigley, 2012; Kaplan & Walker, 2012; Lang, Eisen, & Zivkovic, 2014).
Probiotic supplements may reduce fatigue in mild COVID-19 patients. Probiotic therapy has been shown to reduce digestive and respiratory symptoms, as well as the risk of mortality and admission to the intensive care unit in severe COVID-19 infection (Mey et al., 2023). It's critical to remember regarding obesity which frequently linked to micronutrient deficiencies, which exacerbate the burden of malnutrition. This has detrimental effects on immunological function and skeletal muscle metabolism, leading to an elevated vulnerability to infections and a likely decline in skeletal muscle mass. Obesity patients have an increased risk of acquiring corona virus suffering. and experiencing unfavorable results if they also have multiple sclerosis (MS) or type 2 diabetes mellitus (T2DM). Therefore, it is recommended that healthcare experts, particularly those with expertise in nutrition, provide guidance to these individuals in order to enhance their cardiovascular risk profile (Barazzoni et al., 2022).
IMPACT OF NUTRITION ON IMMUNE SYSTEM
The body's immune response is always active, but it is only when infections are present that its cells become active. The activation of the defence mechanism leads to a notable rise in the demand for components that produce energy, such as amino acids, glucose, and fatty acids. The immunological reaction leads to the production of lipid origin intermediaries, including leukotrienes and prostaglandins, as well as various proteins, such as binding molecules, cytokines, and acute-phase proteins, cytokine receptors, chemokines, and immunoglobulins. The presence of the appropriate precursor like fatty acids and amino acids is a prerequisite for this process. The immune response necessitates substantial cellular proliferation, hence necessitating an increase in the quantity of immune cells accessible for defensive purposes. This process entails the synthesis of DNA, RNA, proteins, and complex lipids, all of which require an ample supply of substrates to facilitate their production. The metabolic processes responsible for energy production and biosynthesis necessitate the presence of specific minerals and vitamins as essential cofactors. Amino acids, such as arginine, serve as precursors to polyamines, which drive genetic material synthesis and division of cells. Nucleotides and nucleic acids rely on the presence of a number of nutrients, including magnesium, iron, folate, zinc. Certain nutrients, namely vitamins A and D, together with their metabolites, have the ability to directly modulate the regulation of genes in immune cells. Nutrients like these play a critical role in immune cell maturation, differentiation, and responsiveness. Innate immunity relies on free radical species to create a pro-oxidating environment. Traditional antioxidant vitamins like vitamins C and E, as well as enzymes that act as antioxidants like glutathione peroxidase, catalase, and superoxide dismutase, help the host protect itself from the oxidative stress caused by free radicals. Essential minerals including iron, copper,selenium, zinc, manganese, are required for the correct functioning of these antioxidant enzymes. Therefore, it is clear that nutrients play a wide variety of roles in supporting the immunological response, highlighting the crucial necessity of a sufficient and well-balanced provision of these substances in order to elicit an effective immunological response. Fundamentally, optimal nutrition establishes a milieu whereby the immune system can effectively and suitably react to many challenges, regardless of their specific characteristics. On the contrary, inadequate nourishment gives rise to a milieu whereby the immune system exhibits suboptimal responsiveness. This phenomenon is well demonstrated in cases of nutritional insufficiency, whether observed in real-life situations or created experimentally. In such instances, there is a notable decline in both inherent and acquired immunity, leading to heightened vulnerability to infections and an exacerbation of their severity. The correction of deficiencies has been found to have a causal association with the reversal of immunological deficits and susceptibility to infection, indicating the importance of particular nutritional availability for immune defenses. Vitamins C, vitamin B12, vitamin B6, vitamin D, vitamin A , Vitamin B9, and minerals like selenium, iron, copper, zinc are among that care for functioning of the immunological response as approved by the European Food Safety Authority. There are several thorough literature studies that examine various elements of the relationship between diet and immunity, with a particular emphasis on the impact of micronutrients (Calder, 2020).Flavonoids encompass a collection of naturally occurring compounds, which may be further classified into distinct subcategories such as flavones, chalcones, isoflavones and flavonols. In addition to their antioxidant effects and antiviral capabilities, these compounds exhibit several other functions. Pectolinarine, Rhoifolin, Herbacetin are three flavonoids that may have anti-coronavirus effects by effectively inhibiting the 3C-like protease, as proved by a recent study by (Jo, Kim, Shin, & Kim, 2020). In addition, it was shown that compounds like helichrysetin, quercetin, herbacetin has the capability to inhibit the enzymatic activity of 3-chymotrypsin-like protease as well as Middle East respiratory syndrome–related coronavirus (Picone et al., 2023).
THE SIGNIFICANCE OF THE GUT MICROBIOTA
The presence of commensal microorganisms in the intestinal tract contributes to the host's immunological defence mechanisms by establishing a protective barrier against the colonisation of infections. Additionally, these bacteria produce proteins that kill bacteria, which have the ability to directly impede the development of microorganisms. There are interactions between commensal microbes and the intestinal epithelium and the immune tissues of the host. The interactions between the host and the bacterium involve the emission of chemical signals or direct cell-to-cell communication. The use of probiotic organisms, specifically Lactobacilli and Bifidobacteria, is suggested as a means to enhance host immunity in response to these activities.Furthermore, several research have explored the effects of probiotic microbes, individually or inconjunction, on defence mechanisms and infection in humans. Certain probiotic organisms have been seen to potentially boost innate immunity, namely by increasing engulf and natural killer cell activity. However, their impact on acquired immunity appears to be less significant (Lomax & Calder, 2009) However, it has been demonstrated in many studies that persons who consume probiotics have enhanced vaccination responses, as discussed in a separate study (Maidens, Childs, Przemska, Dayel, & Yaqoob, 2013). The observed immunological responses indicate that probiotic organisms may have the potential to provide protection against illnesses. Probiotics reduce diarrhea rates and severity, particularly diarrhoea brought on by Clostridium difficile and antibiotic use. It may not come as a surprise that probiotics have an impact on gastrointestinal infections, but they may also offer protection against lung diseases. Studies on mice suggest that the absence of gut bacteria may impair the body's defenses and the prognosis of bacterial or viral respiratory illnesses. Research on probiotics, namely Lactobacilli and Bifidobacterial, has yielded several indications suggesting a decrease in the occurrence of respiratory infections in humans, as well as enhanced results. The existing body of evidence supports the notion that probiotics, particularly Lactobacilli and Bifidobacteria, have the potential to enhance immune function, augment the efficacy of seasonal influenza vaccination, decrease the occurrence of respiratory illnesses, including viral ones, and improve outcomes in individuals with respiratory infections. Consequently, incorporating these microorganisms into a preventive approach may be beneficial in mitigating the likelihood and seriousness of viral infections. Within this particular framework, it has been shown that individuals afflicted with COVID-19 have exhibited intestinal dysbiosis, characterised by decreased quantities of Bifidobacteria and Lactobacilli (Lu et al., 2020; Zuo et al., 2020). In (d'Ettorre et al., 2020) research, COVID-19 patients received a combination of medicines and antimicrobial agents or a comparable treatment with probiotics comprising Lactobacilli, Streptococcus thermophilus, Bifidobacteria. The researchers observed that the group of patients receiving probiotics exhibited improved resolution of symptoms such as diarrhoea and respiratory disease, in addition to other disease symptoms.
The administration of diets containing high levels of omega-3 polyunsaturated fatty acids, such as docosahexaenoic acid, eicosapentaenoic acid, docosapentaenoic acid, fortified with vitamin A, effectively reversed adverse effects on neurotransmitter function, cognition, and behaviour induced by stress in adolescent rats. Furthermore, these dietary interventions were shown to induce changes in the microbiome's makeup. The microbiome, gut, and brain axis describes the two-way communication between the microbiota in the digestive tract and the central nervous system. The aforementioned axis demonstrates significance in the control of cognitive processes and behaviour in animal studies (Bear et al., 2020). A subset of probiotics known as "psychobiotics" affect the central nervous system through metabolic, nervous, humoral, immunological routes. These pathways not only improve the functioning of the gut, additionally they play a role in their anti-anxiety and anti-depressive effects. The gastrointestinal-central nervous system axis is crucial for proper stomach-to-brain communication. The utilization of psychobiotics has drawn the interest of scientists to direct their attention towards a novel domain within the study of neurology, specifically pertaining to a distinct category of probiotics (Cheng, Liu, Wu, Wang, & Tsai, 2019). Certain strains of psychobiotics have demonstrated the ability to mitigate inflammation and reduce cortisol levels, leading to a notable amelioration of symptoms associated with anxiety and depression. Evidence derived from both animal and human research indicates that intestinal microbiome can affect neurological function as well as cognitive development by the synthesis of hormones, immunological components, and metabolites.
Several psychobiotic strains have been identified to treat neurological disorders. These strains include Lactobacillus casei Shirota, Bifidobacterium infantis, Lactobacillus plantarum PS128, Lactobacillus rhamnosus, and Lactobacillus helveticus R0052. These strains have shown promise in alleviating stress-related symptoms. In the context of depression, the strains that have been identified as potentially beneficial include Bifidobacterium bifidum, Lactobacillus acidophilus W37, Lactobacillus helveticus NS8, Lactobacillus helveticus NS8, and Bifidobacterium infantis. On the other hand, when it comes to the treatment of anxiety, the strains that have shown promise are Lactobacillus rhamnosus JB-1, Lactobacillus fermentum NS9, Lactobacillus casei Shirota, and Bifidobacterium infantis, and Bifidobacterium breve 1205. Future research should examine diets that generate centrally active metabolites from bacterial strains that affect brain function. One of the main advantages associated with the utilisation of psychobiotics for maintaining mental well-being in times of emergency like the COVID-19 epidemic is their microbial nature, as their genera are prevalent in digestive tracts. This characteristic potentially offers a lower likelihood of allergic reactions and a decreased dependence on alternative therapeutic interventions, distinguishing them from psychotropic medications (Shabbir et al., 2022).
NUTRACEUTICALS IMPACT ON COVID-19
Polyphenols such as quercetin, resveratrol, and catechins, along with palmitoylethanolamide and N-acetyl-cysteine, have been shown to possess antiviral properties among immunosuppressants. These compounds primarily act by preventing inflammatory pathways, specifically the generation of interleukin (IL-beta) mediated by the NLR Family Pyrin Domain Containing 3 (NLRP3) inflammasome, as well as the secretion of pro-inflammatory cytokines. They also block viral proteases to stop replication (Singh et al., 2021). In addition, it is worth noting that the use of inositol in patients with COVID-19 infection may potentially alleviate the surge of cytokines that is observed, thereby potentially facilitating the overall healing process. Conversely, enhanced inflammation arises as a result of compromised oxidative state. Glutathione supplementation has been shown to enhance the mitigation of damage caused by oxidation in several tissues, particularly in the presence of vitamins and minerals possessing antioxidant capabilities (Silvagno, Vernone, & Pescarmona, 2020). Hence, the combination of glutathione and inositol may serve as a valuable approach for enhancing the inflammatory response and oxidative state in individuals experiencing covid-19 side effects. Lactalbumin, lactoglobulin, lactoperoxidase, serum albumin, and bovine lactoferrin, are being employed to serve as potent immunostimulants, although the mechanisms behind their beneficial effects remain incompletely elucidated. Probiotics, particularly Bifidobacteria as well as Lactobacillus could increase the body's defenses, favoring gut colonization over infections and protecting the intestinal wall, reducing vulnerability to pathogens and their metabolites produced by bacteria (Basak & Gokhale, 2022). Recently, there have been suggestions to utilise certain dietary components as immunomodulators in order to address the therapy for corona virus infection or mitigate lethal effects. The glucan glycophosphopeptide known as glycophosphopeptical regulates both adaptive and innate immunity. The concentrate obtained from Polypodium leucotomos is well acknowledged for its multifaceted impact on several pathways related to the defense against infection. The amino acid glutamine is thought to be absolutely required and has a major role in controlling cytokine release in Covid-19-infected patients (Barrea et al., 2022).
ROLE OF NUTRITION AND SARS COV 2
Some key nutrients that support the immune system include Proteins, vitamin A, B, C, D, E zinc, copper, selenium, Magnesium, Probiotics and Omega fatty acids, Echinacea purpurea, Elderberry, Ginseng. These nutrients can be obtained through a balanced diet or supplementation as represented in Table 1.
COMPLICATIONS ASSOCIATED WITH NUTRITIONAL DEFICIENCY
Carbohydrate consumption stabilises blood sugar and decreases stress through modulating immune cell mobilisation (Alwarawrah, Kiernan, & Maciver, 2018). Bone marrow and thymus T and B cell repertoires are also affected by protein deficiency, which reduces TNF-Alpha and Interleukin-6 generation (McKay et al., 2020). Vitamins and minerals stimulate neutrophil killing, macrophage, innate cell differentiation, and antimicrobial protein production. These nutrients boost adaptive immunity by producing antibodies and memory cells. Lack of macronutrients ( carbohydrates, protein, fat) and micronutrients (trace elements, minerals, vitamins) can impair immune systems and increase bacterial and viral damage. (Chandra, 1996; Shenkin, 2006; Steinbrenner, Al-Quraishy, Dkhil, Wunderlich, & Sies, 2015). Vitamins and minerals deficiency such as magnesium, zinc, iron, and selenium can cause immune insufficiency and infections. In children, vitamin C insufficiency can cause pneumonia, poor immunity, and impaired bone development. For instance, acute respiratory tract illness is linked to low 25-hydroxyvitamin D levels. Vitamin A deficiency affects innate immunity (frequent throat and chest infections), hematopoiesis, and ocular consequences, childhood stunting, fertility issues among women. Insufficient Vitamin B1 causes breathlessness, reflexes, and muscular weakness. Normal-chromic-normocytic anaemia, oxidative stress, inflammation, and cell proliferation result from Vitamin B2 deficiency. Low Vitamin B6 (cofactor of haemoglobin production) reduced oxygen levels in the body. Too little Vitamin D causes rise in viral replication as well as reduced cytokines. Too little vitamin E Inflammation slows child development. Deficiency of magnesium electrons Impaired innate, acquired, and immunoglobulin responses. Low selenium Causes recurrent abortion in pregnant women by mutating harmless RNA viruses (Influenza, Coxsackie) into pathogenic strains. Antioxidant, zinc deficiency T and B cells, antibody synthesis (particularly Immunoglobulin G), and eosinophil concentration were impaired. Repeated abortions in pregnant women stunted foetus development. Iron-deficit Infection response and immune cell growth and maturation are impaired. Childhood cognitive and behavioural issues Acute respiratory infections. Daily meals can include micronutrients that decrease inflammation and boost immunity due to their antiviral properties. By activating macrophages and producing, differentiating, and chemotactic innate immune cells, vitamins and minerals optimise innate immunity (Alam, Bhuiyan, Emon, & Hasan, 2021). A 2020 study found that vitamin D may affect the activity of 70% of SARS-CoV-2 proteins by altering the expression of 25% of human genes producing protein targets (Glinsky, 2020). Deficiency in vitamin D increases susceptibility to COVID-19 infection, morbidity, and death. Regulatory T cells are also a major defence against viral-induced inflammation. Covid-19 patients have low regulatory T cell counts, which vitamin D supplementation may boost (Weir, Thenappan, Bhargava, & Chen, 2020).
Table 1
Nutritional elements essential for treating viral diseases.
S. No | Nutrients | Food Sources | Mode of action against Covid-19 | Biological Importance | References |
|---|---|---|---|---|---|
1. | Proteins | Whole grains, beans, meat, milk, lentils, probiotic yogurt, eggs, fish, Cheese | Essential for cytokine and immunoglobulin production. Sulphur-containing amino acids Increases the radical-hydroxyl neutralising activity of SOD and GSHPx, protecting the host from viral infections. Immunomodulation, antioxidant, neuroprotection | Generates Cytokines and immunoglobulins. Polyamine precursor arginine aids cell development. Antibody production needs plasma arginine. Chemotherapy patients' cell-mediated immunity and antioxidant ability enhanced with Zn and Se-enriched whey protein isolate. In Covid 19 cases, whey protein isolate lowers oxidative free radicals, boosts GSH, and prevents infection. Methionine shortage reduces lymphocyte activity and B and T cell growth and differentiation. Cytokine synthesis requires amino acids. Methionine and cysteine, two sulphur amino acids, are required for the production of interleukin (IL)-1, IL-6, and tumour necrosis factor-alpha. | (Alam et al., 2021; Chen et al., 2020; Chockalingam et al., 2016; Kim, Roszik, Grimm, & Ekmekcioglu, 2018; Tesseraud, Coustard, Collin, & Seiliez, 2008) |
2. | Vitamin A | Eggs, beef liver, cod liver oil, orange and yellow vegetables, fruits, most dark green vegetables, spinach, broccoli. | Antiviral immunity. Regulates immune cell proliferation and differentiation via nuclear retinoid acid receptor, modulating proinflammatory cytokines such TNFα and IL 6. | Immune cell growth and epithelial tissue development. Vitamin A boosts neutrophil phagocytosis and oxidative burst, killing microorganisms. Vitamin A governs CD4+ T lymphocyte and dendritic cell maturation, and its absence alters T helper 1 and 2 lymphocyte balance. T cells home to gut-associated lymphoid tissue with retinoic acid. Some gut immune cells synthesise retinoic acid. CD8+ T cell survival, growth, and antibody production require retinoic acid. Vitamin A regulates the cellular and humoral immune systems and greatly boosted antibody formation following immunisation against viruses. Vitamin A controls immune cell growth, differentiation, and TNFα and IL 6 production through retinoic acid receptor in the nucleus. | (Evans & Mangelsdorf, 2014; Jayawardena, Sooriyaarachchi, Chourdakis, Jeewandara, & Ranasinghe, 2020; Masi et al., 2015; Müller, Svardal, & Frøland, 2000; Ross, 1996; Villamor et al., 2002) |
3. | Vitamin B | Red meat, Dark leafy vegetables, Fruits (bananas, citrus fruits), Brown rice, Cheese, legumes, sunflower seeds and nuts, yogurt, poultry, mussels, fish, eggs, salmon, liver and other organ meats, milk, cheese, oysters, pork. | Serves as a cofactor for metabolic activities, including amino acid degradation and immune modulatory mediator metabolism. These metabolic pathways play a crucial role in viral infection, indicating the need for balanced vitamin intake to regulate the immune response. They control the activity of natural killer cells and cytotoxic CD8+ lymphocytes, contributing to successful virus clearance. | B vitamins regulate digestive immunity and gastrointestinal barrier function.Vitamins B6, B12, and folate boost CD8+ cytotoxic T lymphocyte activity and natural killer cell, aiding virus defence. Pyridoxal phosphate, the active form of vitamin B6, is a coenzyme for many metabolic processes, including amino acid transamination and immunomodulatory mediator metabolism. | (Percudani & Peracchi, 2009; Tamura et al., 1999; Yoshii, Hosomi, Sawane, & Kunisawa, 2019) |
4. | Vitamin C | Cauliflower, Sweet potato, Beef liver, papaya, Oysters, Eggs, broccoli, Citrus fruits, strawberries, tomatoes, pork liver, | Reduce inflammation to prevent cytokine storm. Decrease respiratory infections | Vitamin C maintains epithelium life by synthesising collagen. It also helps leucocyte movement to infection areas, killing microbes by phagocytosis, T lymphocyte function (mainly CD8+ cytotoxic T lymphocytes), natural killer cell activity,and antibody formation. Vitamin C supplementation reduces the length and impact of upper respiratory diseases like the common cold, notably in stressed people. High-dose intravenous Vitamin C helps virus-induced Acute Respiratory Distress Syndrome patients recover from critical lung injury. Vitamin C may help severe COVID-19 since many patients have ARDS. | |
5. | Vitamin D | Seaweeds, oat, soy milk, cereal, Marine fish, beef liver, cheese, egg yolk, milk, shrimp, mushrooms, Cheese | In the respiratory tract, cytokines and TLRs activate vitamin D receptors (VDRs) in many respiratory epithelial and immunological cells. Reduces cold and illness risk Vitamin D induces cathelicidin and defensins to protect respiratory tract tight junctions and destroy enveloped viruses. | Cytokines and Toll-like receptors activate receptors of Vitamin D in a variety of lung epithelium and immune cells. Vitamin D also promotes innate immunity by upregulating VDR in monocytes and targeting the antibacterial protein cathelicidin. Several studies indicated that vitamin D protects against respiratory tract illnesses by activating cathelicidin. Vitamin D also downregulates pro-inflammatory mediators like IL-8, IL-12, IL-6, TNF-α, interferons which participate in cytokine storm. Most immune cells have vitamin D receptors, and some can synthesise pre-vitamin D, indicating that vitamin D may regulate the immune system. Vitamin D improves host defence by increasing epithelium integrity and cathelicidin formation in macrophages and epithelial cells. | (Brahmi et al., 2022; Gombart, 2009; Ilie, Stefanescu, & Smith, 2020; Molloy & Murphy, 2020; Teymoori-Rad, Shokri, Salimi, & Marashi, 2019; Wang et al., 2004) |
6. | Vitamin E | Goose meat Octopus, Marine fish, Soybean oil, sunflower oil, corn oil, wheat germ oil, walnut oil, nuts, seeds, green leafy vegetables (spinach, and broccoli). | Regulate immunological and inflammatory responses, such as T-cell proliferation, granulocyte phagocytosis, and cytotoxicity, via affecting gene transcription. Decline ferroptosis harms lungs, kidneys, liver, stomach, heart, and neurological system. | Antioxidant vitamin E regulates body immunity. Through gene regulation, vitamin E modulates T-cell growth, granulocyte phagocytosis, and apoptosis. | (Alam et al., 2021; Brahmi et al., 2022; Han et al., 2010; Lewis, Meydani, & Wu, 2018; Marko et al., 2007) |
7. | Zinc | soybeans, dark chocolate and cocoa powder , cheese, eggs, red meat, nuts, Oysters, poultry, sesame seeds, beans, pumpkin seeds, lentils, whole grains, dairy products, shellfish. | Inhibits Retrovirus RNA polymerase action and SARS-CoV. Immune modulation and antiviral properties. Decrease COVID-19 infections that inhibit autophagy and enable SARS-CoV-2 RdRp activation in vitro. | Zinc blocks RNA polymerase, which coronaviruses need to reproduce. Zinc ionophorepyrrolidinedithiocarbamate reduced influenza virus replication in vitro and may prevent SARS-CoVreplication.Antiviral defense may depend on zinc-binding metallothioneins. Zinc depletion reduces bone marrow immune precursor cells, thymic atrophy, and naïve B and T lymphocytes. Zinc maintains T and B cell levels. Zinc helps neutrophil external traps catch bacteria. | (Alam et al., 2021; Farzana et al., 2022; Hasan, Rink, & Haase, 2012; Kaushik et al., 2017; Read, Obeid, Ahlenstiel, & Ahlenstiel, 2019; Uchide, Ohyama, Bessho, Yuan, & Yamakawa, 2002; Velthuis et al., 2010; Vignesh & Deepe, 2017) |
8. | Copper | Poultry, rabbit, legumes, nuts, seafood, Viscera, cheese, | Enhancers for SARS-CoV-2 immunity. | Copper is antimicrobial. Copper helps neutrophils, monocytes, macrophages, and natural killer cells. T lymphocytes proliferate and produce IL-2. Copper aids immune cell growth and antiviral reactions. In vitro, thujaplicin and copper chelates suppressed influenza virus-induced death, viral propagation, and cell release. Intracellular copper disrupts influenza viral life cycle. Copper boosts antioxidant state and blood ceruloplasmin, benzylamine oxidase, and superoxide dismutase levels. | (Alam et al., 2021; Brahmi et al., 2022; G, Mark, L, & F, 1997; Li et al., 2019; Miyamoto et al., 1998; Turnlund et al., 2004) |
9. | Selenium | Nuts, pumpkin seeds, mushroom, almonds, wheat bread, turkey, eggs, fish, pork, chicken, beef, garlic, Sea salt, asparagus, sunflower seeds. | Essential for immunological health. Immunostimulates T-cell proliferation, NK cell activity, and innate immune cell activities. | Selenium has protective and anti-inflammatory actions. Selenium supplementation had mixed impacts on influenza cellular defence. Selenium dose-dependently increased T-cell growth and IL-8/IL-10 secretion. | (Alam et al., 2021; Brahmi et al., 2022; Ivory et al., 2017; Rayman, 2012) |
10. | Magnesium | Green leafy vegetables, fruits (banana, avocado),nuts, seeds, legumes, peas, spinach, oatmeal, seafood (Salmon, mackerel, tuna), shrimp, egg, milk, beef, chicken Almonds, black beans, broccoli, brown rice, cashews, flaxseed | Reduces lung inflammation, oxidative stress, and bronchial smooth muscle contraction, promoting bronchodilation. | Magnesium also controls IgG formation and antibody-dependent cytolysis. Magnesium activates many enzymatic processes and is necessary for many physiological functions. Magnesium regulates C-reactive protein, IL-6, NF-κB immune networks. | (Alam et al., 2021; Brahmi et al., 2022; Liang, Wu, Huang, Jiang, & Lin, 2012; Tang, Ding, Jiao, Wu, & Kong, 2020; Wallace, 2020) |
11. | Probiotics | Yogurt, curd, Sauerkraut, fermented soybean paste. | Inhibit SARS-CoV-2 major protease, S1 glycoprotein, and ACE. Probiotics and macrophages collaborate to produce interleukin-12, which triggers interferon-γ production, a key antiviral cytokine. | Enterococcus faecalis, live Bacillus subtilis and Lactobacillus rhamnosus GG reduced ventilator-associated pneumonia compared to saline. Lactic acid and antimicrobial proteins from natural probiotic bacteria and commensal bacteria can directly prevent parasite growth in addition to forming a physical barrier. Certain probiotic organisms appear to boost innate immunity but have less of an impact on acquired immunity. Probiotics or prebiotics boost adult antibody reaction to seasonal influenza inoculation. The probiotic lactobacillus paracasei(CBA L74) helps keep dysentery at bay. Probiotics and synbiotics like Lactobacillus acidophilus LB and Lactobacillus rhamnosusGG lessen diarrhea duration, hastens recovery. Probiotics lessen the likelihood of antibiotic-caused diarrhoea in people aged eighteen to sixty four years old, but not in those over the age of 65. Bacterial spread and secondary illness can be reduced by microecologics. Reduce bowel harmful bacteria, toxin generation, and gut microfloradysbiosis illness. In mice, gut microbiome reduction impairs immune responses and worsens respiratory infection outcomes. | (Brahmi et al., 2022; Clarke, 2014; Jafarnejad et al., 2016; Lei, Shih, Liu, Lin, & Yeh, 2017; Li et al., 2019; Lomax & Calder, 2009; Malagón-Rojas, Mantziari, Salminen, & Szajewska, 2020; Morrow, Kollef, & Casale, 2010; Thomas & Versalovic, 2010; Yang et al., 2019; Yeh et al., 2018; Zeng et al., 2016; Zhang & He, 2015) |
12. | Omega 3 fatty acids | Canola oil, Shrimp, Walnuts, spinach, oysters, marine fish, soybeans. | Preventing viral invasion by altering cell bilipid membrane lipids. Anti-inflammatory, vasodilatory, and platelet-anti-aggregatory. Reduce inflammation and boost phagocytosis. | Docosahexaenoic acid (DHA) and Eicosapentaenoic acid (EPA) reduces inflammatory eicosanoids from arachidonic acid, NF-κB signaling, and inflammatory cytokines. By altering cell bilipid membrane lipids, omega-3 fatty acids may inhibit viral entry. Omega-3 regulates acquired and innate immunological reactions and inflammation processes. | (Brahmi et al., 2022; Calder, 2013; Calder, 2015; Calder, 2017; Hathaway et al., 2020) |
13. | Echinacea purpurea | Echinacea purpurea species (aqueous and ethanolic extract of whole plant) | Inhibitors of virus entrance, internalisation, and replication. Immunomodulatory activity | Echinacea dramatically decreased interleukin (IL-1-β) and TNF-α expression. Echinacea purpurea could alleviate inflammation by synergistic biological stimulation of Cannabinoid receptors, moderate fatty acid amide hydrolase inhibition, or endocannabinoid transport. Anti-inflammatory, immune-modulatory, and antiviral, properties are owing to polyacetylenes, polysaccharides, volatile-terpenes, caffeine acid esters, phenolic compounds, alkamides, and glycoproteins. | |
14. | Sambucus nigra (Elderberry) | Fruits of Sambucus nigra species | Inhibition of ACE2 and SARS-CoV2 RBD binding. SARS-CoV2 inhibition. | Elderberry regulates pro-inflammatory cytokines, making it antiviral against several infections. Plant-derived caffeine inhibits coronovirus spike protein binding to angiotensin converting enzyme 2 receptors, making it anti-coronaviral. Phenolic acids, flavonols, Anthocyanins,are major phytoconstituents. | |
15. | Ginseng | Ginseng roots | Targets cytokine storms, anti-viral processes, immune regulation, and inflammation reduction. Decreases SARS-CoV-2 replication in the cell and reduces viral RNA (vRNA) copies. | Ginseng reduces Covid-19 by decreasing inflammation and boosting antiviral defence. Major gingeng components are saponins, Ginsenosides, Triterpene glycosides. |
Table 2
Nutritional requirements and intake per day for Covid-19 affected population
S.No. | Nutritional Requirements | Recommended daily dose (Intake per day) for diseased population | Significant health outcome in Covid-19 | References |
|---|---|---|---|---|
1. | Vitamin C | 1-2g/day | Lessening of cases of upper respiratory illness | |
2. | Fish oil (omega-3polyunsaturated fatty acids and docosahexaenoic acid) | 2-4 servings/week or 40-80g/day | Alzheimer's disease, metabolic syndrome, gastrointestinal cancer, coronary heart disease, and dementia attenuate. | |
3. | VitaminD3 | 10,000 IU/day (250 µg/day) | Lower rates of acute respiratory infections | |
4. | Vitamin E | 60 to 800 mg/day | Proven effective in the treatment of pneumonia | https://ods.od.nih.gov/factsheets/COVID19-HealthProfessional/#h41 |
5. | Zinc | 30–50 mg/d | Limiting the Spread of RNA Viruses like influenza and corona | |
6. | Copper | 7.8 mg/d | Modulates immunological response by decreasing oxidative stress | |
7. | Echinacea | 2,400 mg Echinaforce (E. purpurea preparation) | Antiviral activity (including coronaviruses) | |
8. | Elderberry | 175-mg lozenges Elderberry ; 600–900 mg Elderberry capsules | Anti influenza activity A decrease in the number of upper respiratory symptoms associated with colds and viruses | |
9. | Selenium | 1000–1600 μg/day | Immune stimulant, anticoagulant, anti-apoptotic, and antiviral efficacy for the treatment or prevention of COVID19 | |
10. | Magnesium | 332mg/day | Mineral with anti-inflammatory properties that helps to reduce inflammation and oxidative damage during times of high cytokine activity | |
11. | Proteins | 1.5 -2.5 g | Protein supply may limit muscle protein breakdown for gluconeogenesis, preventing further catabolism during viral infection. | (Brugliera et al., 2020; Moonen, Hermans, Jans, & Zanten, 2022) |
12. | Vitamin A | 25 000 IU/d oral vitamin A | Effectiveness in alleviating COVID-19 symptoms including fever, body soreness, weakness, and fatigue decreased dramatically. | |
13. | Panax ginseng (Korean ginseng) | 3 g of Korean Red Ginseng tablet/day | Rapidly produces Corona virus antibodies. Increase COVID-19 vaccination efficacy by regulating cytokines and chemokines and immunological cell proliferation and activity. | |
14. | Probiotics | Probiotic Bifidobacterium longum [2g/ sachet, 1 sachet two times/ day (4 g/day)] Probiotic lactobacilli Lactobacillus plantarum [1g sachet, 1 sachet/day (1 g/ day)] | Increased serum IgA Common cold symptoms reduced | |
15. | Vitamin B12 | 500 μg | Helps treat macrocytic anaemias, pernicious anaemia and reduces COVID-19-related organ damage and symptoms. |
A summary table of nutritional requirements and intake per day for affected population is explained in Table 2.
NUTRITIONAL RECOMMENDATION IN DIFFERENT AGE GROUPS
The first trimester of pregnancy has the same estimated energy demands as nonpregnant women, while the second trimester adds 340 calories and the third 452. Increase in weight in pregnancy is lower for overweight and obese women compared average-weight women (Rasmussen & Yaktine, 2009). Nevertheless, it is important to note that nutritional and lifestyle variables have the potential to not only directly impact fertility but also exert an influence on the susceptibility to several disorders that might hinder fertility. These diseases include polycystic ovarian syndrome, endometriosis, and uterine fibroids. Several studies have indicated that there may be a potential association between high-dose vitamin C (at a dosage of 750 mg/d) and a combination of arginine, iron, and antioxidants supports in facilitating expectant mothers (Agarwal, Gupta, & Sharma, 2005). It is recommended that women who are at risk of becoming pregnant should consider supplementing their diet with a daily intake of 400 mcg of folic acid in order to decrease the likelihood of birth defects. Additionally, it is important for these women to ensure that they maintain sufficient levels of vitamin B12 (De-Regil, Peña-Rosas, Fernández-Gaxiola, & Rayco-Solon, 2015). In the male population, infertility can arise due to an imbalance in the synthesis of oxygen radicals by semen and oxygen-radical scavengers disrupts equilibrium. This occurrence can arise as a result of smoking, infection of the reproductive system, varicocele, and potentially due to inadequate dietary habits. The findings from controlled trials indicate that the administration of potent combinations of additional antioxidants, such as vitamins C (at doses exceeding 200 mg/d), vitamin E (at doses ranging from 200 to 600 IU/d), and selenium (at doses ranging from 100 to 200 μg/d), have demonstrated positive effects. These effects include improvements in sperm motility and morphology, as well as enhanced pregnancy rates, with a particular emphasis on individuals who were formerly smokers (Agarwal, Nallella, Allamaneni, & Said, 2004). Women who are pregnant or breastfeeding need more macronutrients and micronutrients. Insufficient diets could elevate the child's likelihood of developing chronic diseases years later. Early prenatal starvation increased adult weight, heart problems, and neurological abnormalities (Clair et al., 2005; Kyle & Pichard, 2006; Roseboom et al., 2001). Pregnancy requires 1.1 g/kg/d of protein for foetal development and milk production. However, protein source may be as essential as amount. Some data shows that vegetable protein may be safer than animal protein. Arachidonic acid, a precursor of prostaglandin E2, cholesterol, saturated fat, and edible microbes are abundant in meat (Mechanick & Brett, 2002). Pregnant and nursing women need more vitamins A, C, E, and B vitamins (niacin, folate, riboflavin, pyridoxine, cobalamin, and thiamine, choline). Folate should be ingested in sufficient levels before conception to prevent neural tube abnormalities. (Das et al., 2023) Pregnant women need more selenium, copper, magnesium, molybdenum, phosphorus, iron, potassium, chromium, manganese, calcium and zinc (Siega-Riz, Bodnar, & Savitz, 2002). There are higher nutrient needs per kilogramme of body weight during infancy and childhood compared to other stages of development. As cells divide rapidly during growth, they need energy, protein, and nutrition for the production of DNA and protein, calorie, and fat metabolism. For older infants, specifically those aged 7-12 months, the Recommended Daily Allowance (RDA) for protein is 1.2 grammes per kilogramme per day, equivalent to 11 grammes of protein per day. Children aged 1-3 years have an RDA of 1.05 grammes per kilogramme per day or 13 grammes of protein per day, while children aged 4-8 years have an RDA of 0.95 grammes per kilogramme per day or 19 grammes of protein per day (Institute of Medicine, 2005). Infants have greater per-kilogram fatty acid needs than adults. The central nervous system relies on the essential role played by long-chain fatty acids, specifically docosahexanoic and arachidonic acid. These fatty acids are synthesized from linolenic as well as alpha-linolenic acids through the processes of enzymatic reactions. Young children and infants shouldn't eat saturated fats because they delay neuronal development (Ascherio & Willett, 1997). Micronutrient requirements for people 19–50 years of age vary somewhat by sex. Vitamins C, K, B1, B2, and B3, as well as choline, magnesium, zinc, chromium, and manganese, are especially important for men. When compared to males of the same age, women who menstruate have a greater iron need (Lanou, Berkow, & Barnard, 2005). Older people have lower energy needs than younger people do since they are less active and have lower lean body mass. To combat osteoporosis due to age and fracture, the Dietary Reference Intake (DRI) for vitamin D is raised from 600 IU/d in those 19–70 years old to 800 IU/d in those > 70 years old. Because iron is conserved and losses are reduced in postmenopausal women, the recommended daily intake of iron drops from 18 mg in women aged 19–50 to 8 mg/d (Institute of Medicine, 2005). It is still crucial to guarantee enough protein consumption for older individuals, even when low-protein diets have been linked to health advantages including lower rates of diabetes, cancer, and overall mortality among persons younger than 65 (Levine et al., 2014). Ageing and illness can cause a decline in a person's ability to chew, swallow, digest, and absorb nutrients, making it difficult for some seniors to meet their nutritional needs (Chernoff, 2005). Selenium is an essential element for proper immune system function, and a recent research found that many elderly people living in long-term care facilities were deficient in it. As a result, vulnerability to infections and cancers increases with compromised immune function. Enhanced vitamin B6 intakes for the elderly are supported by the fact that the vitamin plays a function in immunity (Institute of Medicine, 1998).
AFTER-COVID-19 TREATMENT ALTERNATIVES
One of the most important strategies in the fight toward the covid-19 disease is prevention. The utilization of biologically produced compounds is a potential substitute for preventative care, since it can augment the body's defenses in the prior contact stage. Research has demonstrated that the adoption of diets that include plants can exert a favorable influence on the makeup and functionality of commensal bacteria residing in the gastrointestinal tract, hence fostering overall well-being of the intestinal microbiota. Curcumin, the principal chemical compound found in Curcuma longa L., demonstrates activity against corona viruses, and possesses protective effect against oxidation of cells. The alkaloid component piperine, which is obtained from the plant Piper nigrum L., is being observed to augment the innate immune response by facilitating IFN-1 mRNA expression and interferon regulatory factor 3 phosphorylation. Garlic, a prophylactic strategy, may relieve symptoms in covid-19 infected people. Aloin and aloe-emodin, the main components of Aloe vera are potential antiviral compounds. These compounds limit the replication of virus or destroy the lipid coating to kill enveloped viruses such as corona viruses. Ajowan essential oil isothymol is protective against viruses as well as antimicrobial in action. Endosome lysosomes contain Cathepsin L. (CatL), which damages the framework of the cell, allowing the spike protein in corona virus to bind and enter cells that are being attacked. The discovery of botanicals and phytonutrients that suppress CatL might be a major treatment goal for corona virus suffered patients. Natural remedies may help prevent and treat the covid-19 pandemic. Scientists may employ these strategies in the difficult context of developing drugs to treat covid-19 (Das et al., 2023).
CONCLUSION
The current investigation examined the significance of proper diet in individuals with covid-19, establishing the connection between nutritional intake, immunity, ageing, malnutrition, obesity, gut microbiota, nutritional deficiency, and nutritional recommendations. It has become evident that this association has assumed a critical function during the covid-19 pandemic, throughout the many stages of the illness, especially among individuals who are more susceptible to encountering adverse consequences, such as those who are obese, undernourished, over nourished and of advanced age. A well-balanced and nourishing dietary regimen assumes a pivotal significance in the recovery process of persons afflicted from COVID-19, particularly individuals encountered with cardiovascular or lung problems, alongside individuals with debilitation and consequential weight loss and frailty. These patients require personalized dietary assistance, initiated promptly throughout their treatment, which is adequate and appropriately timed to facilitate optimal metabolic utilization in order to promote recovery. The immune response is influenced by several elements, among which diet plays a significant role. Sufficient nutrition has a pivotal role in enhancing the immunological response. The body’s defense mechanism may experience impairment in elderly individuals, particularly among those who exhibit frailty, obesity, malnutrition, and inadequate intake of micronutrients. Nutritional insufficiency is also associated with abnormal chronic inflammation and oxidative stress, which contribute to the onset of debilitation as well as increase the risk of poor outcomes in the context of infection. The potential correlation between inadequate nutrition and the immune system, particularly its inflammatory aspect, could potentially elucidate the heightened susceptibility to severe outcomes of corona virus infection observed in elder individuals and obese persons. Proper food helps promote a diverse gut flora, which boosts the immune system. The gut microbiota is affected by a number of factors, including aging and obesity. While there are various interventions, such as utilizing dietary supplements, adopting a particular nutritional regimen, and implementing similar measures, that show potential in preventing, managing, and aiding in the recovery of individuals with corona virus, stressing the importance of crucial data derived from randomized clinical trials to substantiate these claims. The current body of evidence regarding the relationship between the microbiota and the interaction between nutrition and brain activity is expanding. Notably, animal studies have yielded compelling results. However, it is important to note that this area of investigation is still in its nascent phase. Therefore, it is crucial to further explore the potential benefits and applications of this discovery. This research could lead to advancements in various industries, such as medicine, technology, and environmental sustainability.